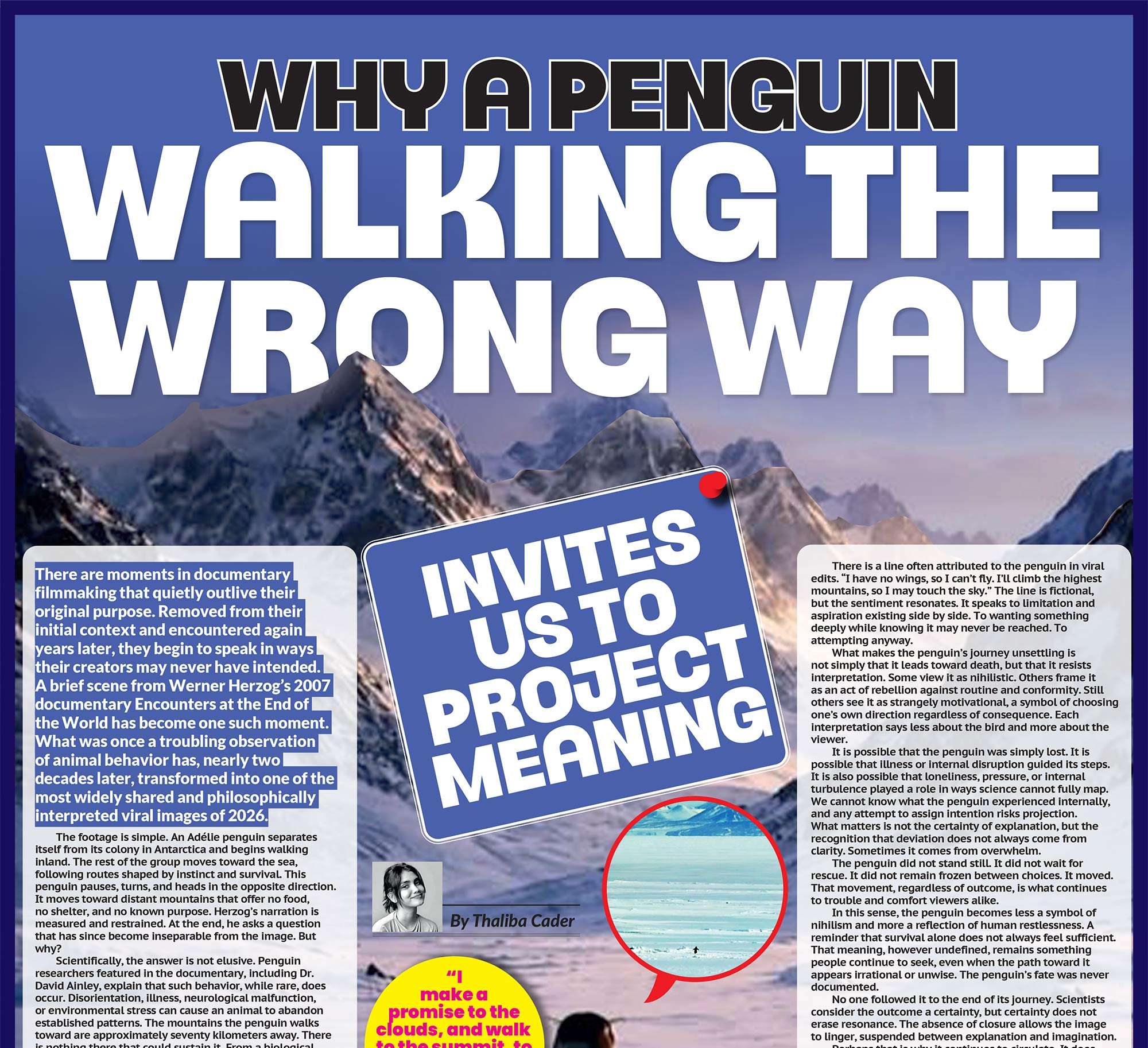
The thyroid is one of the smallest organs in the human body, yet its influence reaches almost every system that keeps us alive and functioning. Shaped like a butterfly and located at the base of the neck, this modest gland plays a central role in regulating metabolism, energy production, heart rate, body temperature, digestion, reproductive health, and cognitive function. It produces two key hormones, thyroxine and triiodothyronine, which act as messengers that determine how quickly or slowly the body’s cells operate. When the thyroid functions well, it works quietly in the background. When it does not, the effects can be widespread, disruptive, and deeply misunderstood.
Despite its importance, thyroid disease remains one of the most under recognised and under diagnosed health conditions globally. Millions of people live for years with persistent symptoms that interfere with daily life without ever receiving a clear explanation. Fatigue that never seems to improve, weight changes that feel impossible to control, anxiety without an obvious trigger, or a persistent mental fog are often treated as isolated issues rather than signs of an underlying hormonal imbalance. The thyroid problem we keep missing is not simply medical. It is also cultural and systemic, shaped by limited awareness, diagnostic gaps, and a tendency to dismiss symptoms that do not present dramatically.
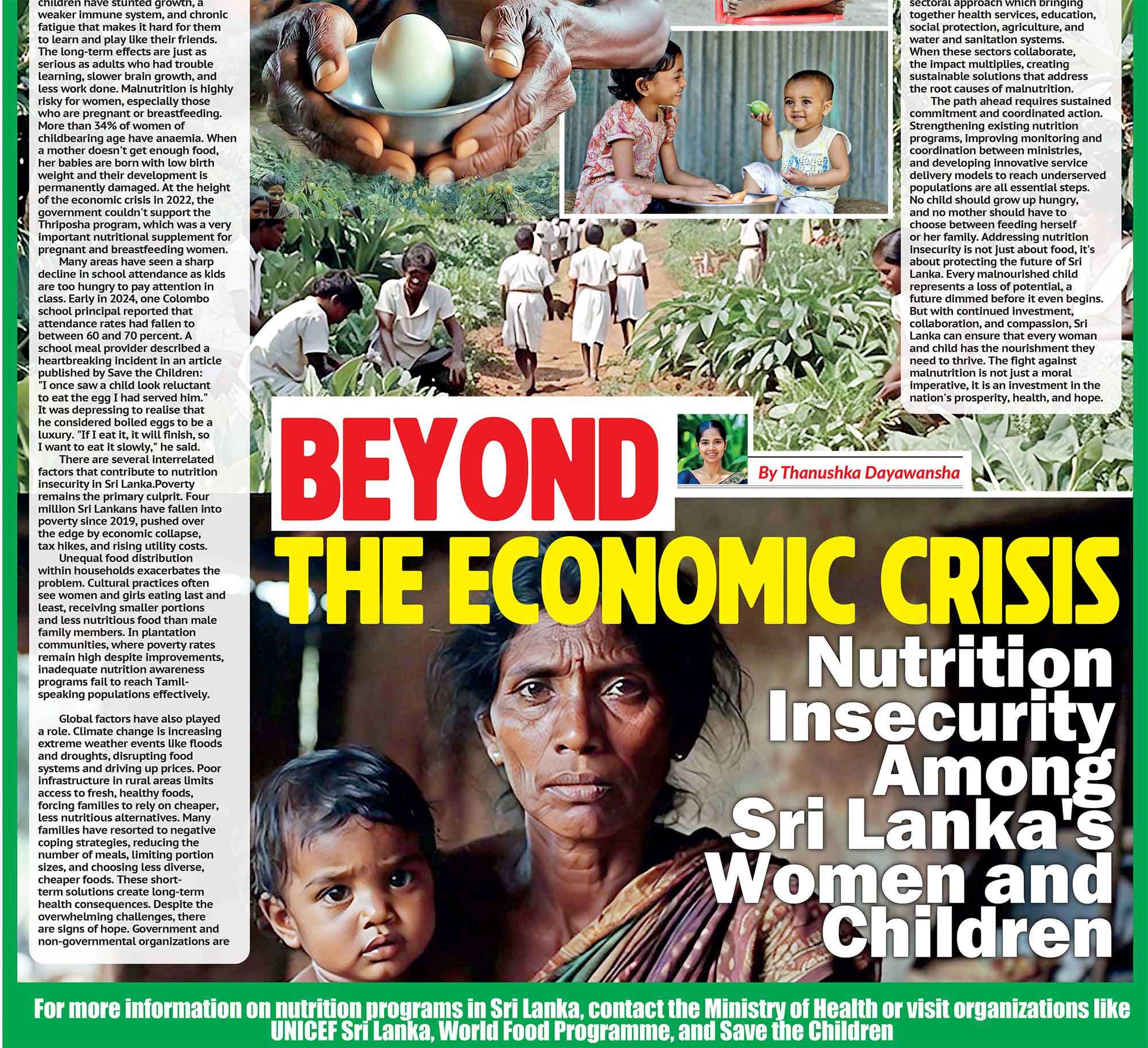
One of the main reasons thyroid disorders go unnoticed is the way they develop. Hypothyroidism, which occurs when the thyroid does not produce enough hormones, typically progresses slowly. Symptoms often appear gradually and inconsistently. People may feel constantly tired despite adequate rest, gain weight without changes in diet or activity, feel unusually sensitive to cold, experience dry skin or hair thinning, struggle with constipation, or notice a decline in concentration and memory. These symptoms rarely appear all at once. Instead, they accumulate over time, making them easy to attribute to stress, ageing, overwork, or lifestyle habits.
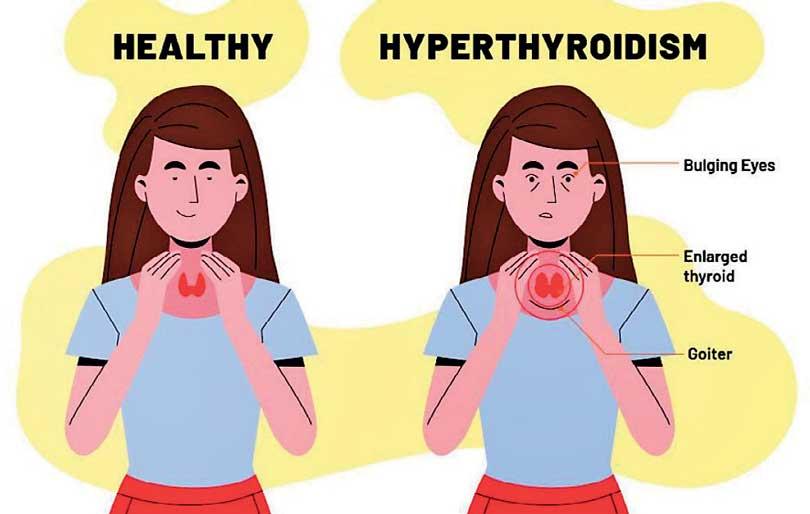
Hyperthyroidism, on the other hand, involves excessive hormone production and can feel more intense. Symptoms may include rapid heartbeat, unexplained weight loss, tremors, excessive sweating, irritability, anxiety, and intolerance to heat. Yet even these signs are frequently misinterpreted. Because they overlap closely with anxiety and panic disorders, many patients are treated for mental health conditions before an endocrine cause is ever considered. In both cases, the thyroid remains overlooked while symptoms are managed in isolation.
Thyroid disease also shows a strong gender bias. Women are far more likely than men to develop thyroid disorders, particularly autoimmune conditions. Hormonal shifts during puberty, pregnancy, the postpartum period, and menopause increase susceptibility to thyroid dysfunction. Autoimmune thyroid diseases such as Hashimoto’s thyroiditis and Graves’ disease are especially prevalent among women. In these conditions, the immune system mistakenly targets the thyroid gland, either gradually destroying it or overstimulating hormone production.
This intersection between the immune system and the endocrine system adds complexity to both diagnosis and treatment. It also exposes long standing issues in how women’s health is approached. Symptoms such as fatigue, weight fluctuation, mood changes, and brain fog are often normalized or dismissed, particularly in women, as emotional or psychological rather than physiological. When thyroid disease presents subtly, it fits easily into this pattern of dismissal, delaying diagnosis and prolonging suffering.
Diagnostic practices themselves pose another challenge. Thyroid disorders are usually identified through blood tests that measure thyroid stimulating hormone and thyroid hormone levels. While this appears straightforward, it often fails to capture the full picture. Routine health screenings do not consistently include thyroid testing unless symptoms are severe or clearly indicative of thyroid dysfunction. Even when tests are performed, results that fall within broad reference ranges are frequently considered normal, even if the individual continues to experience significant symptoms.
This reliance on laboratory thresholds creates a gap between numerical values and lived experience. Many people are told their thyroid function is normal despite feeling unwell, leaving them without answers or effective treatment. Others begin treatment but continue to struggle, only to be reassured that their test results look fine. This disconnect highlights the limitations of a purely numbers-based approach and points to the need for more nuanced, patient centered care.
The long-term consequences of untreated or poorly managed thyroid disease are significant. Chronic hypothyroidism has been linked to cardiovascular disease, elevated cholesterol levels, infertility, menstrual irregularities, depression, and cognitive decline. In pregnancy, untreated thyroid dysfunction increases the risk of miscarriage, preterm birth, and impaired neurological development in the fetus. These outcomes are not rare and are largely preventable with timely diagnosis and appropriate treatment.
Hyperthyroidism carries its own risks when left unmanaged. Persistent excess thyroid hormone places strain on the heart, increasing the likelihood of arrhythmias and heart failure. Bone density may decline, leading to osteoporosis and fractures, while muscle weakness and fatigue can undermine physical health. In severe cases, a thyroid storm, marked by an abrupt surge in hormone levels, can be life threatening. These risks underscore the importance of early detection and ongoing monitoring.
Treatment for thyroid disease is generally effective but requires careful management. Hypothyroidism is commonly treated with synthetic thyroid hormone replacement, while hyperthyroidism may involve antithyroid medications, radioactive iodine therapy, or surgery. Finding the correct treatment and dosage is rarely immediate. Hormonal needs change over time, influenced by age, stress, pregnancy, and overall health. Both insufficient and excessive treatment can cause harm, making regular follow up essential.
A common frustration among patients is the persistence of symptoms despite achieving test results that are considered normal. This has prompted growing recognition that thyroid care must extend beyond laboratory values alone. While blood tests are essential, they should not override how a person feels or functions. A more holistic approach that considers symptoms, quality of life, and individual variability is crucial for effective long-term management.
Environmental and nutritional factors also influence thyroid health. Iodine deficiency, although less widespread than in the past, still contributes to thyroid dysfunction in certain populations. Chronic stress, inflammation, exposure to endocrine disrupting chemicals, and nutrient imbalances can all impair thyroid function or worsen existing disease. These factors highlight that thyroid disorders do not exist in isolation but are shaped by broader biological and environmental contexts.
Perhaps the most overlooked aspect of thyroid disease is its impact on daily life. Living with an undiagnosed or inadequately treated thyroid condition can affect productivity, relationships, and emotional wellbeing. Many patients describe feeling disconnected from themselves, less capable, less energetic, and less sharp than they once were. Because symptoms are often invisible and difficult to measure, patients may struggle to be taken seriously, leading to feelings of frustration and isolation.
At its core, the thyroid problem we keep missing is about more than hormones. It reflects how healthcare systems respond to subtle illness, how symptoms are validated or dismissed, and how patient voices are heard. The thyroid may be small, but its influence is profound, and overlooking it comes at a real human cost.
Recognizing the signs of thyroid dysfunction earlier, improving diagnostic awareness, and adopting more personalized treatment strategies are essential steps forward. As research continues to explore the connections between hormones, immunity, metabolism, and mental health, thyroid disease stands as a reminder that the body’s quiet systems deserve as much attention as its most obvious ones.
Improving thyroid health outcomes requires more than medication alone. It demands better education among healthcare professionals, routine screening for high-risk groups, and public awareness that treats endocrine health as essential rather than optional. Most importantly, it requires listening to patients, especially when symptoms persist despite normal test results.
As modern lifestyles become more demanding and environmental pressures increase, thyroid disorders are likely to rise rather than disappear. Addressing them early, with scientific precision and genuine empathy, can prevent years of silent suffering. In doing so, we restore not only hormonal balance but also quality of life, clarity, and a sense of being heard to those who have spent too long searching for answers.