- Medical accuracy verified by a Consultant Clinical Oncologist
Cancer is one of the leading causes of death worldwide, yet it is also one of the most preventable and treatable diseases when detected early. Across the globe, health experts emphasize that early detection can transform cancer outcomes by improving survival rates, reducing the severity of treatment, and preserving quality of life. This World Cancer Day on February 4, the importance of screening, awareness, and timely medical intervention is underscored, reminding individuals and communities that early detection is one of the most powerful tools in the fight against cancer.
Early detection refers to identifying cancer at an initial stage, often before symptoms appear or when tumors are still localized and easier to treat. It involves a combination of screening programs, self-examination, and prompt medical attention for unusual symptoms. Unlike late-stage diagnosis, which often requires aggressive treatment and carries a lower survival rate, early-stage cancer can be addressed with more effective and less invasive interventions. According to the World Health Organization (WHO), early detection not only improves survival but also significantly reduces the economic and emotional burden of cancer on individuals, families, and healthcare systems.
One of the most compelling reasons to prioritize early detection is the clear evidence linking it to survival. For example, breast cancer detected through mammography at Stage I has a five-year survival rate of approximately 99 percent, compared to significantly lower rates when diagnosed at later stages. Similarly, cervical cancer identified through routine Pap smears or HPV testing can be treated effectively before it becomes invasive. Precancerous polyps can be easily identified through stool tests and colonoscopy, and removal of these polyps can prevent the development of colorectal cancer. These examples demonstrate that screening and vigilance save lives and highlight the critical role of awareness campaigns in educating the public.
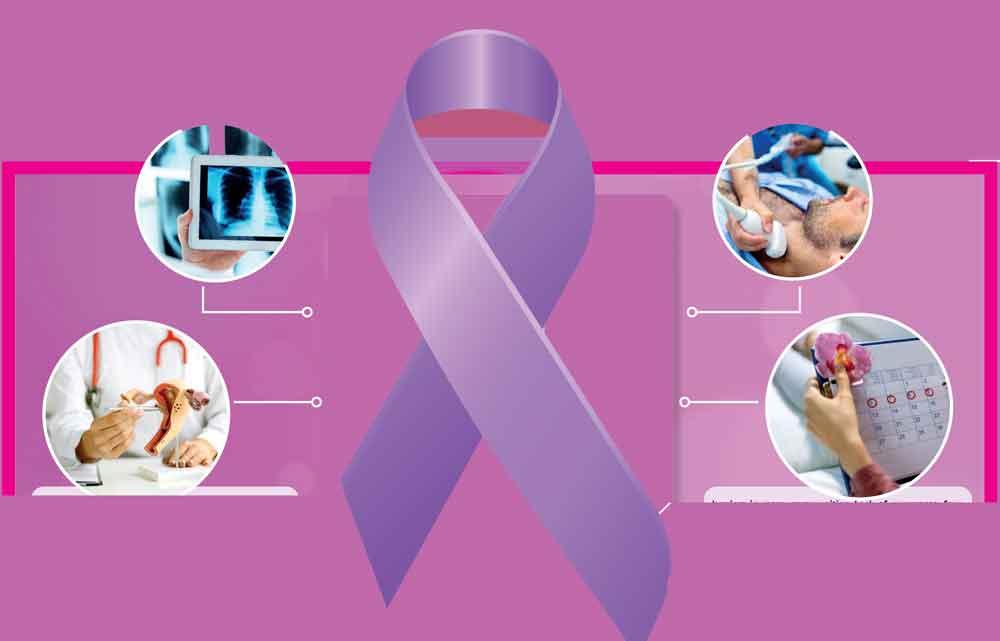
Understanding which screenings are appropriate requires knowledge of risk factors, age, and family history. Health professionals recommend different screening tests for men and women depending on their risk profile:
Breast Cancer: Women aged 50 and above are encouraged to undergo regular mammograms, while self-examinations can help detect unusual changes at any age, especially among younger women. Those with additional risk factors may require alternative screening methods.
Cervical Cancer: Pap smears and HPV testing are essential for sexually active women of any age. Vaccination against HPV at a younger age drastically reduces the risk of developing cervical cancer later in life.
Colorectal Cancer: Adults over 45 are advised to undergo colonoscopy or stool-based screening, with frequency determined by risk factors. Early detection identifies polyps before they transform into malignant tumours.
Prostate Cancer: Men, especially those over 50 or with a family history of prostate cancer, may benefit from PSA testing. Decisions about screening should be made in consultation with a healthcare professional.
Early detection is not limited to these cancers. Self-examination of the oral cavity using a torch and mirror is very useful in identifying suspicious areas. Oral cancer is the most common cancer among men in Sri Lanka. Skin, liver, and lung cancers also benefit from vigilance and timely intervention. While melanoma screening is emphasized in European countries, it is extremely rare in Sri Lanka. Individuals with a history of hepatitis or heavy alcohol use are advised to undergo regular liver monitoring. Similarly, people at high risk of lung cancer, such as long-term smokers, may benefit from low-dose CT scans.
Equally important as structured screening is self-awareness. Knowing one’s body and recognizing changes can facilitate early diagnosis. Symptoms such as unexplained weight loss, persistent cough, unusual bleeding, lumps, skin changes, or prolonged digestive disturbances should never be ignored. While these symptoms do not always indicate cancer, seeking prompt medical advice ensures timely evaluation and reduces the risk of late-stage diagnosis.
Despite the clear benefits, early detection faces barriers in many communities. Lack of awareness, fear, stigma, and limited access to healthcare often prevent individuals from seeking screening. In our culture, stigma remains a major obstacle. Fear of diagnosis can delay action, while myths and misinformation create confusion. Public health campaigns play a crucial role in overcoming these barriers by providing education, normalizing conversations around cancer, and emphasizing the benefits of proactive care.
Economic and infrastructural challenges also limit access to screening. This is one reason Sri Lanka does not have a widespread breast cancer screening programme using mammography, as facilities within the Ministry of Health are limited. In low- and middle-income countries, the lack of screening facilities, high costs, and shortages of trained healthcare providers hinder timely diagnosis. Governments, NGOs, and community organizations are working to expand screening programs, subsidies tests, and train healthcare workers to reach underserved populations. Mobile screening units, telemedicine consultations, and community outreach programs have proven effective in increasing access and awareness, particularly in rural areas.
Beyond medical benefits, early detection empowers communities socially and psychologically. Individuals who undergo regular screening are more likely to adopt other preventive measures such as healthier lifestyles and vaccination. Communities that prioritize awareness foster environments of shared responsibility, where people support one another in seeking care, discussing symptoms openly, and reducing stigma around cancer. Education campaigns in schools, workplaces, and community centers ensure that knowledge reaches younger generations, instilling habits that reduce long-term risk.
Technology is revolutionizing early detection. Innovations in diagnostic imaging, biomarker testing, and artificial intelligence are improving accuracy and accessibility. Digital tools enable risk assessment, symptom tracking, and appointment scheduling, making screening more convenient and less intimidating. AI-assisted imaging can detect anomalies that may be missed by human observation, allowing for earlier intervention. Mobile health applications also provide reminders for routine checks, educational resources, and access to telehealth consultations.
Mental health and emotional support are closely linked to early detection. Fear and anxiety about testing or a possible diagnosis often prevent individuals from seeking care. Counselling, patient education, and empathetic communication by healthcare providers help reduce these fears. When people feel supported and informed, they are more likely to participate in regular screenings and encourage loved ones to do the same.
It is also important to recognize that early detection is part of a holistic approach to cancer prevention. Alongside screening and vigilance, lifestyle factors must be addressed. Betel chewing, particularly among men from lower socio-economic backgrounds, is a significant risk factor that requires targeted education beyond English-speaking communities. Combining screening with healthy diets, physical activity, tobacco cessation, and vaccination maximizes prevention and improves outcomes.
Early detection also reduces the economic and social burden of cancer. Late-stage cancers often require intensive, prolonged, and expensive treatment, causing financial hardship and emotional strain not only for patients and families but also for the healthcare system. When cancer is identified early, treatment is typically simpler, less invasive, and more effective, allowing individuals to maintain productivity and minimize disruption to family life and work.
Finally, early detection fosters a culture of proactive health management. Individuals who are aware of risks and engaged in screening programs are more likely to participate in preventive healthcare throughout their lives. World Cancer Day awareness campaigns inspire people to prioritize regular check-ups, vaccination, symptom monitoring, and open conversations about health concerns. This culture of vigilance benefits entire communities by creating networks of support, advocacy, and empowerment.
In conclusion, early detection of cancer is one of the most effective strategies for reducing mortality, preserving quality of life, and minimizing the physical, emotional, and financial burdens associated with the disease. It is a shared responsibility among individuals, healthcare providers, policymakers, and communities. Through education, accessible screening, awareness campaigns, and supportive care, cancer can be identified at its earliest stages, enabling timely intervention and improved outcomes.
On this World Cancer Day, let us recognize the impact of early detection and commit to proactive health practices. By catching cancer early, we are not just treating a disease; we are saving lives, empowering communities, and creating hope for a healthier future.